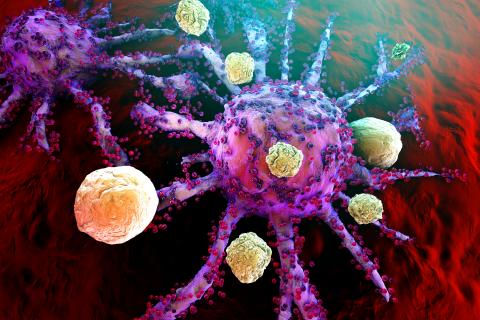
Cancer is a daily battle for many, and for decades chemotherapy has been the frontline’s best defense. That is changing thanks to increasing research in the fields of immunology and genetics. Scientists may have discovered the ultimate secret weapon in the battle against cancer: a patient’s own immune system.
Immunotherapies such as Chimeric Antigen Receptor T-Cell therapy, or CAR-T, are changing the prognosis of cancer so rapidly that the industry is scrambling to keep up. New therapies require doctors to become experts overnight. Hospitals need new state-of-the-art equipment. Patients must weigh the risk of unknown side effects against the risk of dying from cancer. Despite the literal life or death stakes, the results of these treatments are altering the way we treat cancer, and with it, the healthcare industry.
In the midst of it all, commercial health and Medicare Advantage plans are facing a new fight regarding how to cover the cost of these ever-evolving treatments.
Industry Shake Up
Commercial health and Medicare Advantage plans currently rely on prior authorizations using the FDA label to determine patient access. In the Medicare space, the Centers for Medicare and Medicaid Services (CMS) have agreed to pay for CAR-T therapy for patients who meet strict requirements. However, that will change come 2020, and both commercial health and Medicare advantage plans are weighing their options.
HIRC’s research shows that a majority of commercial health and Medicare Advantage plans favor using prior authorization according to the FDA label to determine CAR-T therapy coverage for diffuse large B-cell lymphoma. As competition begins to increase in the space, both types of plans favor covering all products at parity, followed by designating the most cost effective product as preferred. Medicare Advantage plans report that they would most likely manage patient access based on NCD criteria from CMS, though some uncertainty remains regarding how to manage patient access to CAR-T and other immunotherapies. Both commercial health and Medicare Advantage plans report that they would also like to see risk/outcomes-based contracts to assist with managing the costs of CAR-T therapy or other novel contracting approaches.
HIRC’s research shows a trend towards insurers covering all products at parity in the near future. Still, concerns remain. Currently, CAR-T therapy is available only at select hospitals nationwide. Commercial health plans worry about limited sites of care, expanded indications, combinations, cost, and the quickly evolving nature of CAR-T and immunotherapies in general. Medicare Advantage plans cite concerns regarding limited sites of care, lack of long-term data, and overall cost.
Emerging Therapies
Despite the challenges that come with implementing new therapies, the future is bright for immuno- and gene therapies in oncology.
Recently, scientists from the University of Pennsylvania revealed that they are studying the use of CRISPR gene editing technology in patients with cancer. Should CRISPR be approved for the treatment of cancer, it would allow doctors to modify patients own immune cells in a lab before reintroducing the genetically altered cells back into the body. CRISPR is considered an improvement upon CAR-T therapy because it allows “living drugs” to multiply faster and attack cancer more aggressively.
The hope is that CRISPR technology can be used to treat a larger variety of cancers than CAR-T, which is currently used only for leukemia and lymphoma. For now, scientists remain cautiously optimistic. In the first safety test, CRISPR modified cells did not produce any adverse effects while fighting cancer in the trial patient group.
While the industry grapples with a changing treatment landscape, one thing remains clear: new immunotherapies could give patients more than a fighting chance in the battle against cancer.

